NEW DELHI: Researchers have identified a neurochemical signature that sets Parkinson’s disease apart from essential tremor—two of the most common movement disorders, but each linked to distinct changes in the brain.
In a new study in Nature Communications, scientists from Virginia Tech’s Fralin Biomedical Research Institute at VTC and the College of Science identified unique chemical signaling patterns of two key neurotransmitters—dopamine and serotonin—that distinguish these two disorders.
“This study builds on decades of work,” says Read Montague, a scientist at the Fralin Biomedical Research Institute and a co-senior author, who with colleagues developed the multifaceted technologies and the theoretical constructs for the work over their 15 years at the research institute.
“From adapting behavioral game theory into something that functions like a medical test to refining machine learning models that can see brain chemistry in real time, we’ve always aimed to translate insights into something clinically useful,” says Montague, who directs the Center for Human Neuroscience Research at the institute. “This study takes a clear step in that direction.”
The researchers focused on a brain region involved in decision-making and reward processing—the caudate of the striatum.
Using a machine learning-enhanced electrochemical technique during deep brain stimulation (DBS) surgery on essential tremor and Parkinson’s patients, the team measured fast fluctuations as patients played a game involving fair and unfair offers—a task designed to understand decision-making and brain chemistry.
In an early study to emerge from this work in 2018 and published in Neuropsychopharmacology, researchers revealed the first-ever recordings of simultaneous sub-second fluctuations of dopamine and serotonin during active decision-making in a conscious human subject.
The early breakthrough laid the groundwork for the latest.
“The data had been collected as long as eight years ago by Montague and his team at the research institute and their collaborators at Wake Forest University, but we came back at it with better tools and a fresh perspective—and finally saw what was there all along,” says William “Matt” Howe, assistant professor with the School of Neuroscience in the College of Science and co-senior author.
During DBS surgeries in 2017 and 2018, Wake Forest University neurosurgeons Adrian Laxton and Stephen Tatter helped perform the recordings using carbon fiber electrodes in Parkinson’s disease and essential tremor patients while they played a game where they accept or reject offers.
The research protocol was carried during a part of the surgery where the neurosurgeons already monitor brain activity in real time to precisely locate a small target area of the brain for electrical stimulation to treat the symptoms of the disorders.
Now, in the Nature Communications study, researchers applied a computational model to track how those patients formed and adjusted their expectations during the game, revealing signature chemical signaling patterns tied to each disorder.
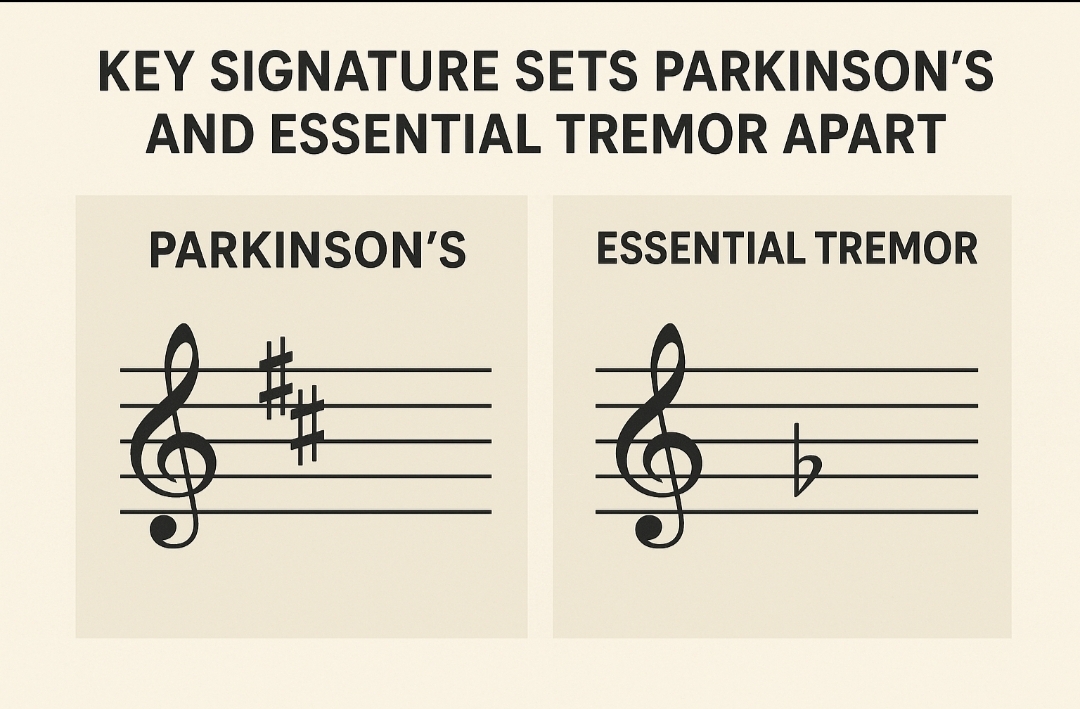
In people with essential tremor, monetary offers that violated their expectations during the game triggered a seesaw pattern—dopamine levels rose, while serotonin dropped. This oppositional response—with one neurotransmitter rising as the other fell—mirrored patterns seen in earlier studies of brain activity during decision-making.
In the latest findings, this reciprocal neurochemical signaling was absent in patients with Parkinson’s disease.
It’s known that dopamine-producing neurons die in Parkinson’s disease, so researchers expected dopamine to be the clearest chemical difference in the brain.
But when they looked closely—using refined tools and a model of how people formed expectations—it was not dopamine that best distinguished Parkinson’s from essential tremor. Instead, it was serotonin, a different neurotransmitter that has not been as prominent in theories of Parkinson’s disease, opening a new view and potentially powerful scientific and clinical insight into this disease.
“What surprised us was how much serotonin stood out,” Howe says. “It wasn’t just that dopamine was disrupted, which was expected. It was that the normal back-and-forth between dopamine and serotonin was gone. There’s neither the serotonin dip nor the dopamine rise. It’s not just one system being disrupted—it’s the lack of that dynamic interaction that turned out to be the clearest difference between Parkinson’s and essential tremor.”
The computational model followed a form of machine learning known as reinforcement learning, which gradually improved its ability to detect patterns as it processed more data from past experiments. Earlier work from Montague and colleague Terry Lohrenz established the importance of this process at the level of neurons and behaviour, setting the groundwork for this new series of experiments and analyses.